A million child deaths around the world can be prevented. It would take a big mobilization of health care workers and small packets of nutritional food.
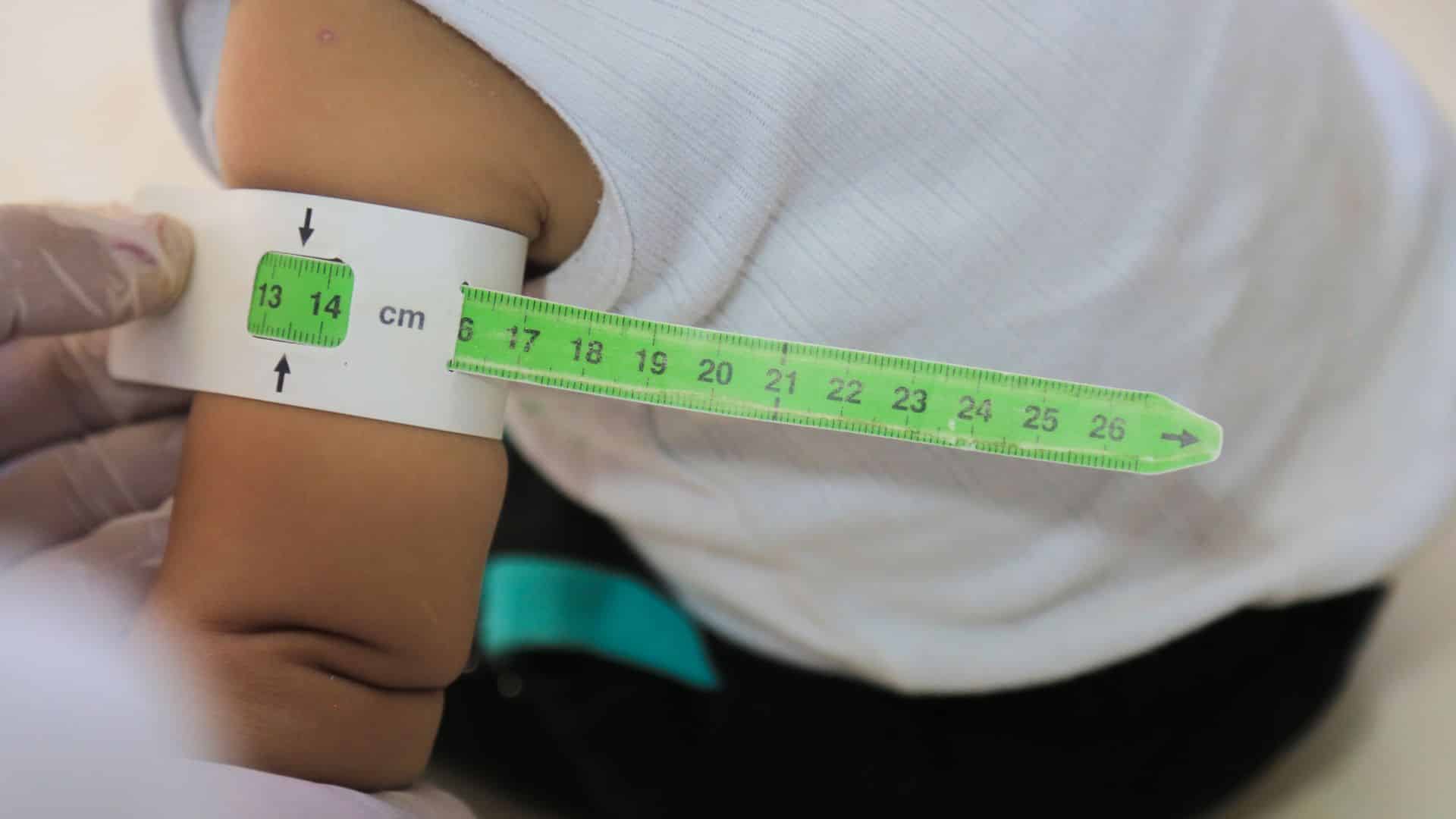
A doctor examines a child for malnutrition by measuring the mid-upper-arm-circumference. Credit: Mohammad Bash
About one million children around the world die of severe malnutrition. But international health organizations say these deaths could be largely prevented with help from a combination of low-cost nutritional packets and an army of community health workers alongside other key child health actions.
Some 45 million children have what’s known as “wasting”, a serious form of malnutrition defined by extremely low weight relative to a child’s height. Some 13.6 million children have severe wasting — which puts them at a risk of death of more than 11 times higher than that of healthy children.
And there are a huge number of children who experience nutritional oedema, another severe form of malnutrition that often goes unrecorded.
But most children who have severe wasting or oedema can be successfully treated at home with ready-to-use therapeutic food packets that typically include peanut paste, milk powder, sugar, oil and vitamins and minerals.
A child with severe wasting can recover in six to eight weeks, on average, with a treatment of about 150 packets of the ready-to-use food. This could vary with the weight of the child.
People in the community who help save children
Community health workers — who live in the community and can provide basic health care needs without needing the formal education of a nurse or doctor — could be trained to provide this treatment.
In Pakistan, for example, community health workers, known there as Lady Health Workers, are already key players in reaching children, said Dr. Rozina Khalid, a nutrition consultant and physician in Pakistan.
“Community health workers are actually the backbone of our community, already providing health services,” Khalid said. “Why not utilize the same people who are already working on health and have knowledge?”
These health workers already provide services such as vaccinations and infant and young child feeding counselling in many places. Khalid believes there is potential for these workers to help with wasting and oedema.
The United Nations identified lowering the number of children who have wasting as part of its Sustainable Development Goals — a blueprint for peace and prosperity around the planet. But the COVID-19 pandemic, climate change and humanitarian crises have derailed years of efforts to tackle wasting.
According to UNICEF, five million children with severe wasting or oedema were treated in 2020, but for every child who received treatment, two more children were missed.
The Global Action Plan on Child Wasting, a collaboration between United Nations agencies to address wasting and oedema, reported that the number of wasted children who can access treatment is still unacceptably low.
Life-saving food in small packets
Back in 2007, UNICEF and other U.N. agencies endorsed a plan called Community-Based Management of Acute Malnutrition that revolutionized the way that severe wasting and oedema are managed.
It aimed to increase the number of children accessing treatment, prevent deaths and lower costs to families whose children were admitted to hospitals.
The approach involved training and supporting community health workers who could identify children who have wasting and oedema and connect them to treatment and access to the ready-to-use therapeutic food and antibiotics.
This year for the first time, World Health Organization guidelines on the prevention and management of wasting and nutritional oedema recommend that community health workers treat children with wasting and oedema who don’t need to be admitted to hospital in some places if certain conditions are met.
UNICEF estimates that the the ready-to-use treatment costs about $100 per child. It was projected to increase by 16% over a six-month period in 2022. That, in turn, would likely result in fewer children accessing this essential product.
Food as medicine
Because ready-to-use-food has not been considered medicine, health systems might not order and stock it the way they do antibiotics and vaccines.
In response, the World Health Organization added it to the Model List of Essential Medicines for Children this year.
Khalid says that most technical experts have wanted it to be included in this list – and believes it “will work wonders.”
A 2021 report by Emergency Nutrition Network found that community health workers are seen by many to be essential to scale up the treatment of severe wasting and oedema. And researchers in Mali found that mobilizing community health workers can be cost-effective and lower the costs to families affected by wasting and oedema.
However, they must have enough training and be supervised regularly for this to be done, according to the WHO guidelines. Khalid said that because the work is hard and time-consuming, community health workers should also be financially compensated.
Unfortunately, this is not always the case. A 2023 review published in The Lancet found that NGOs commonly exploit unpaid or underpaid community health workers. The consequences include damaging their well-being and that could mean compromising the care of children.
“We need to look into more details of how to do it more effectively,” Khalid said.
Questions to consider:
- What is child wasting?
- What are some challenges in providing ready-to-use therapeutic food to needy communities?
- Do you think of food as medicine? Why or why not?

Allison Daniel is a researcher and journalist with a focus on global health and nutrition. She holds a PhD in nutritional sciences with a specialization in global health from the University of Toronto.
Read more News Decoder articles about world health:
